A Promising Breakthrough in Lung Testing for LAM Patients: Introducing Oscillometry
At The LAM Foundation, we believe that hope grows through research—and today, we’re excited to share a new advancement that could transform how we monitor lung health in individuals with LAM.
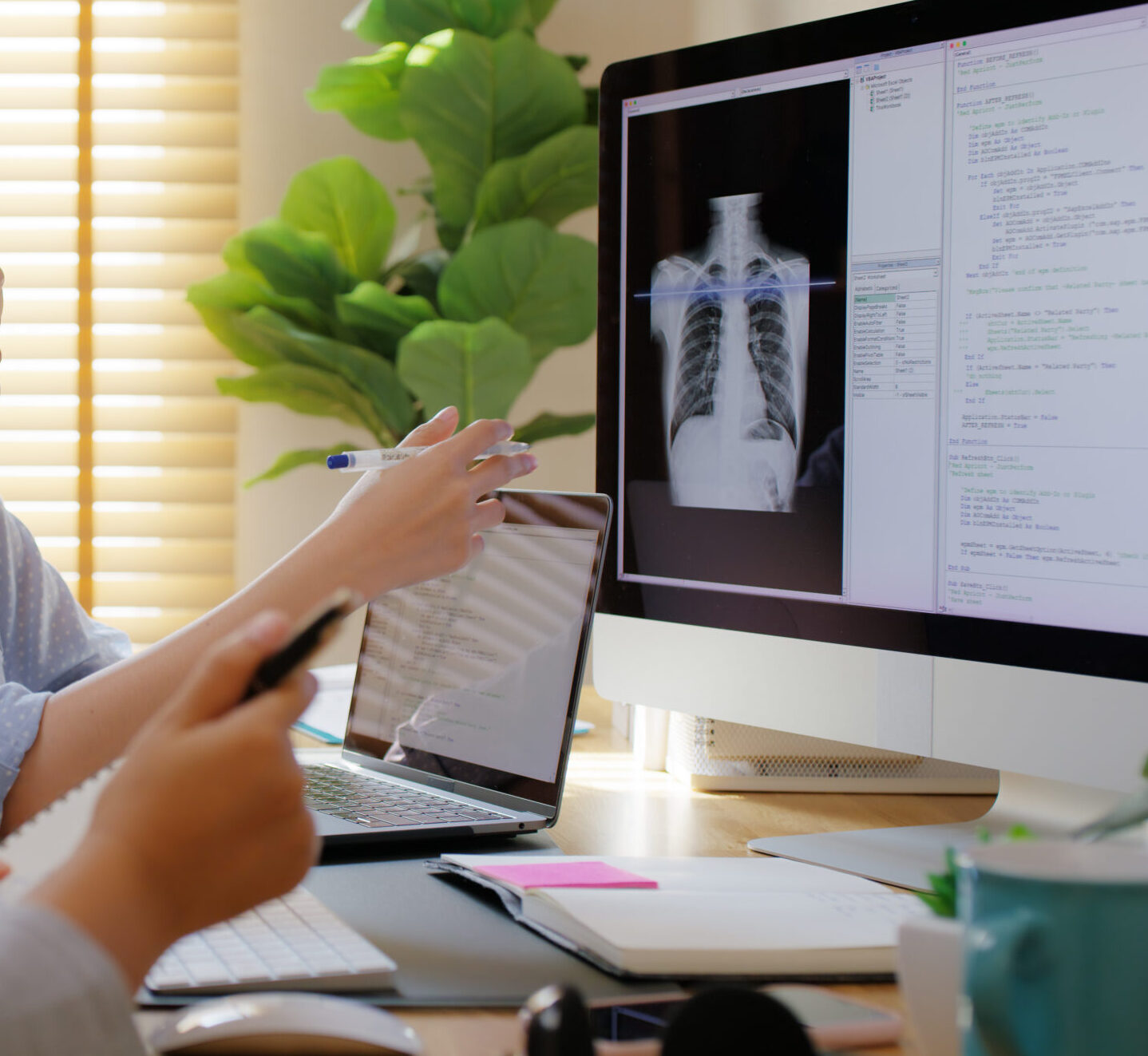
For years, pulmonary function tests (PFTs) like spirometry and plethysmography (also known as “the body box”) have been the standard tools to measure how well the lungs are working. These tests are incredibly valuable—but they also have limitations. They require patients to breathe forcefully or sit in specialized equipment that’s only available in large centers. And sometimes, they can miss early signs of lung decline.
But now, thanks to research funded by The LAM Foundation, we’re exploring a simpler, more sensitive, and patient-friendly option: oscillometry.
What Is Oscillometry?
Oscillometry is a new way of measuring lung function—and it’s as easy as breathing.
Unlike traditional tests that require forceful effort, oscillometry works while you’re just breathing normally. It only takes about 10 minutes, is non-invasive, and may be able to pick up changes in the lungs sooner than other tests can.
This is a huge step forward—and one that brings new hope for earlier detection and better monitoring in LAM.
What Did the Study Show?
With support from The LAM Foundation, Chung-Wai Chow MD, PhD, FRCPC at the University of Toronto conducted a pilot study comparing oscillometry to standard PFTs in 50 women with LAM and 49 healthy volunteers.
Here’s what they found:
- The traditional tests (spirometry and body box) showed similar results in both groups.
- But oscillometry revealed clear differences and was able to detect signs of lung function abnormalities in the LAM group that the standard tests completely missed.
This means oscillometry could uncover lung changes before they show up in other tests to provide a new window into what’s happening in the lungs, earlier than ever before.
Why This Matters
This test is a new opportunity.
- For patients, it means a quick, comfortable, and easy way to monitor lung health.
- For doctors, it provides a more sensitive tool to catch changes early and personalize care.
- For the LAM community, it’s a sign that research is moving forward—with real, meaningful impact.
Most importantly, it represents the power of patient-funded research. Without your support, this study would not have been possible.
What’s Next?
This exciting discovery is just the beginning. Researchers plan to follow LAM patients over time to see if changes in oscillometry can predict disease progression—which could help guide treatment decisions even earlier.
Dr. Chow hopes this work will inspire more LAM clinics around the world to adopt oscillometry in both research and patient care.
Ready to help move us closer to a world without LAM? Donate today.