I Am a LAM Patient and Oxygen Advocate. Here’s Why Congress Needs to Pass the SOAR Bill.
Bev Jackson is one of the leading LAM community advocates for passing SOAR (Supplemental Oxygen Access Reform) legislation. Her interview has been edited for length and clarity.
TLF: Please explain when you were diagnosed with LAM and when you had to go on supplemental oxygen, as well as any other treatment.
BJ: It all started in 2000 when I was getting extremely short of breath while playing tennis. My primary care physician prescribed an inhaler which gave me no improvement. For the next five years, I continued to ask my doctors for a solution. In 2003 I nearly had the diagnosis when a pulmonologist said I could possibly have lymphangioleiomymoatosis (LAM), but she ruled it out because it normally didn’t happen in post-menopausal women like me. But she did prescribe oxygen for exercise. Then, in 2005, I met a woman who had LAM and exercised using oxygen. I was thrilled to find out my symptoms sounded like hers. That woman was our own Cindy Beasley! I was introduced to The LAM Foundation and Dr. Frank McCormack, who looked at my CT scans and said it sure looked like LAM. In 2009, I enrolled in the MILES Trial that was testing if sirolimus would slow the progression of LAM. Within two weeks, I had improvements in my breathing and was able to reduce my continuous flow rate. Then in 2019, I participated in the RESULT Trial to see if the combination of sirolimus and resveratrol would show more improvement. The two together let me reduce the rate of flow of my continuous oxygen once again. Now, after nearly 20 years, I am stable with supplemental oxygen, sirolimus, and resveratrol. I don’t do things as well as I did 20 years ago but I am living a very active life!
TLF: How did oxygen and having LAM change your day-to-day life?
BJ: This is how I dealt with my diagnosis of LAM. Since writing this, I find that my feelings parallel what the researchers say are the steps in dealing with grief: denial, anger, bargaining, depression/grief, acceptance. However, I only felt that I had three steps.
Phase One of Dealing With LAM: Why me?
This was the phase of educating myself about LAM. I called the LAM Foundation and got the LAM Handbook. I didn’t tell them I thought I had LAM; just ordered the booklet. Guess that is denial? I read it from cover to cover. During this phase, I did a lot of soul-searching. It was the first time it had hit me that life does not go on forever. I thought a lot about my life. I came to peace with myself. I knew I had lived a full life and I could face death.
Phase Two: Adjustments in my life.
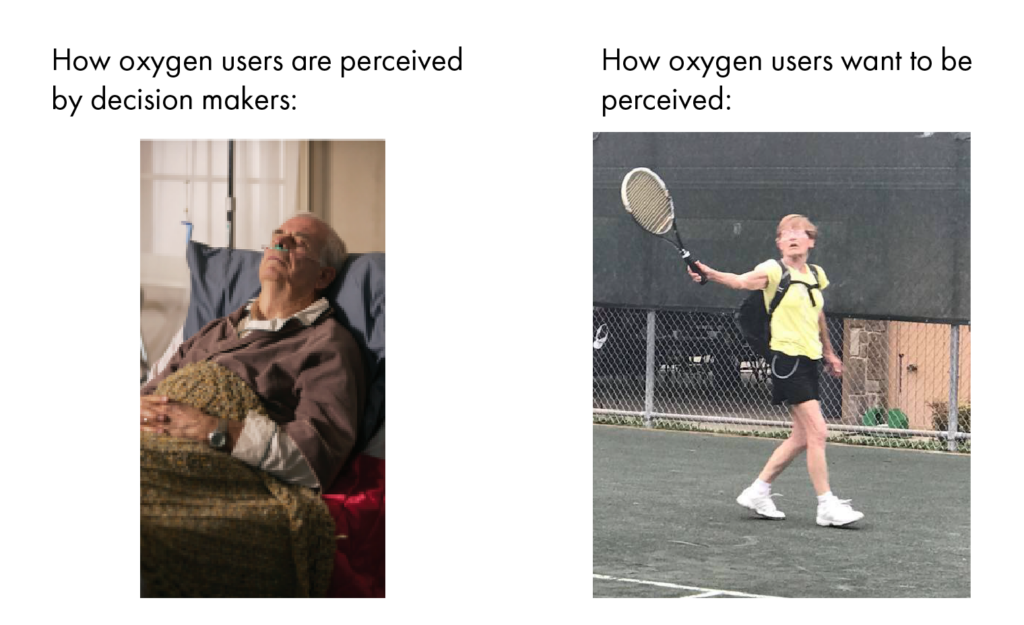
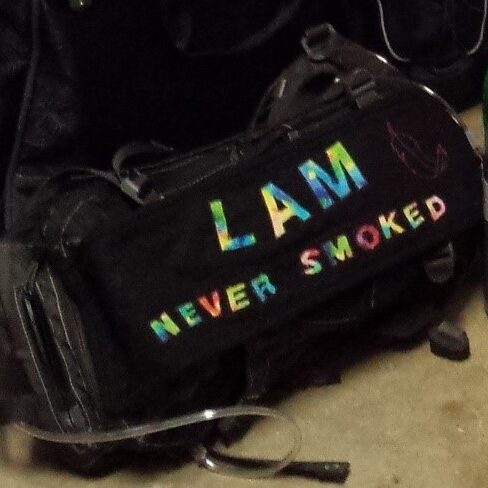
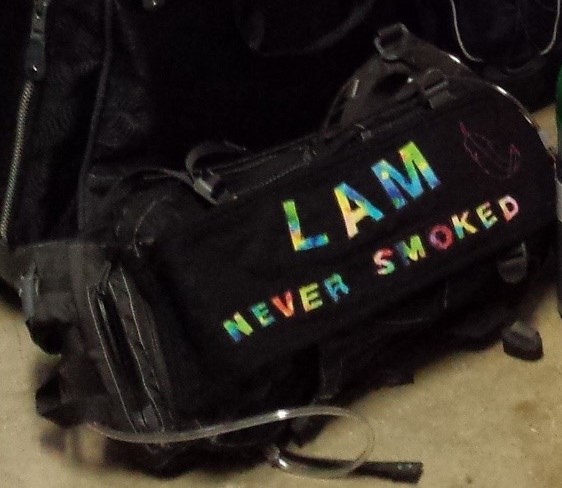
Accept that I have limitations. Can’t play every match in a weekend tennis tournament. Can’t take long hikes. Can’t ski. Use oxygen!! Don’t be embarrassed by what people will think. It bothered me that people think I use oxygen because I smoked. So, I made a “banner” that is stuck to my oxygen backpack that says: “LAM. Never smoked.” It has opened doors for people to ask me about my disease. And I can help raise awareness about LAM.
Phase Three: Just keep on living.
After several months nothing new happened. No lung collapses. My breathing wasn’t significantly worse. I was still doing everything I used to do. Just not doing it as well or as fast. I understand the Spoon Theory. Set priorities on what you will do. My priorities are set by how much oxygen it takes to do things. Do things in smaller sections. Don’t try to clean the whole house in two hours. Tackle the bathroom one day. Vacuum one room the next day. Mow the yard. Rest. Blow off the driveway. Rest. Trim some bushes. Rest. A new concept for me!
My breathing is slowly declining. I have to go back to Phase 2 and do new adjustments to what I can do. I am stubborn. So, it is difficult to admit the adjustments are necessary. It usually just means accepting that oxygen is needed for more activities.
There are times I say sure I will do so and so. Then I realize I will need oxygen to do that. Hiking, for example, there’s no way I can go for a whole day hike. It is nice to know that I can briefly forget that I need to use so much oxygen.
But I will not give in to it. I will live my life to its fullest—with my backpacks of oxygen!
TLF: What does the outside world not understand about the challenge living with supplemental oxygen?
BJ: The planning that goes into everything you do. How many tanks of oxygen will it take to do activities? Are there going to be stairs where I am going? Is there going to be a hill or even slight incline that will require oxygen? How long will I be outside the house?
To take a vacation this is a checklist that I have to go through:
- Make plane reservations.
- Follow up with the airlines to let them know that I will be using oxygen while flying.
- Work with my local oxygen supplier to get oxygen tanks and a concentrator delivered to my destination.
- Follow up with the local oxygen supplier to be sure that the request has been honored at my destination.
- Coordinate with my destination to be sure someone will be available when the oxygen is delivered.
- Be sure to pack regulators and cannulas because you never know if the destination oxygen supplier will provide those items.
I hate flying because of all the uncertainties of getting the oxygen at the destination. I prefer road trips so I can pack all the oxygen I need. No stress! This is what the back of my car looks like when all of my oxygen is loaded for a road trip.

TLF: You’re something of an oxygen advocate. What does that mean?
BJ: First, I want LAM women to be educated about supplemental oxygen before they need it. The scenario that most (including me) describe is that they knew nothing about oxygen when they were given the prescription. The oxygen arrives at your house with no education. I want others to know there are options for the kind of equipment. They need to know which will best fit their needs.
When LAM women have questions about oxygen, I have been more than excited to answer their questions. I try to explain the differences between pulse and continuous flow delivery systems so they can understand the choices they need to make. I have seen too many women purchase pulse only POCs only to find out their oxygen needs outlive the device they purchased.
I have a whole wish list of things I want to change about oxygen. At the top of that list is a “portable” device that will be lightweight (no more than 5 pounds), at least 5 liters continuous flow, and batteries that will last at least 2 hours at 5 liters continuous flow. Dr. Joel Moss from the NIH led in getting a grant for such a device researched and funded through NIH. I was lucky to work with Dr. Moss, Patricia Ortiz, and Mary Stojic in the initial stages of writing the specifications for such a device. Although this device has not yet been produced, I have great hopes that sometime in the future it will be available.
You can’t be an advocate for changes in the world of oxygen without getting involved in trying to make changes to “rules” that affect oxygen. That leads to lobbying Congress for changes.
TLF: For those who don’t know about SOAR, what is it and why is it important?
BJ: SOAR stands for Supplemental Oxygen Access Reform. It is the name given to the bill that has been introduced into both the Senate and House to make changes to oxygen. The basic problem is that people who need supplemental oxygen are not given the type they need nor the amount they need. The bill addresses four main issues:
- Change “home oxygen” to “supplemental oxygen” to more clearly represent the requirements needed to live full lives outside the primary residence.
- Ensure access to liquid oxygen for patients for whom it is medically necessary.
- Create adequate reimbursement for respiratory therapists so patients have access to their expertise.
- Establish standardized documentation for prescribers to use that will ensure adequate reimbursement and protect against fraud.
People who require supplemental oxygen have not been guaranteed the type of equipment or the amount of oxygen needed for their disease. This bill will remove competitive bidding for supplemental oxygen so oxygen suppliers will be reimbursed appropriately.
TLF: What would you like to see happen in terms of getting women access to and reimbursement for supplemental oxygen?
BJ: The items that are in the SOAR bill would cover it.
TLF: This doesn’t just affect LAM patients. How big is the advocacy community around the SOAR campaign?
BJ: The American Thoracic Society has a special interest group made up of professionals (and patients) that support patients with all types of lung diseases. This group is the one that put together the SOAR bill and got it introduced into Congress. Some of the organizations that are represented in this Special Interest Group are The COPD Foundation, The American Lung Association, The LAM Foundation, The Pulmonary Fibrosis Foundation, The Pulmonary Hypertension Association, The American Association of Respiratory Care, Running With Air, and The American Thoracic Society.
In addition to the large Special Interest Group, there is a small group of five patients that the grassroots advocacy organization of the American Lung Association guides. We are the ones who have gotten patients to write their stories to be presented to members of Congress and signed patients up to be on a Zoom call with legislators.
TLF: Describe the efforts of other LAM patients in lobbying Congress for SOAR. Many have gone out of their way to tell their stories. How big is the group?
BJ: LAM women have been more than willing to share their stories to move this issue forward. After sharing their stories, they were then asked to participate in a zoom call with targeted Senators and Representatives to impress on them the importance of sponsoring the SOAR bill. Ones that participated in this effort (and I hope I haven’t overlooked anyone) are Susie Picart, Helen Grice, Joyce Dillon, Karen Kinsey, Lynette Weese, Nancy Saphier, Sarah Morgan, Susan Poole, Terri Rice, Carol Ann Laugavitz, Ally Venugopal, Sharon Rich, Sally Nagel, Marla Hamlin, Pat Rubadeau, Barb Hawkins, and Marcy Sachs.
Other LAM patients who have participated in meetings with their legislators on behalf of SOAR include Beth Daugherity, Ali DeChristopher, Steph Dreyer, Sarah Poitras, Mary Stojic, Abigail Passeri, Elizabeth Zampino, and Cindy Beasley.
Pattie Goodman needs to be recognized for her daily Facebook posts during 2024 Worldwide LAM Awareness Month. She educated everyone, not just Lammies, on what is necessary to lead a full life while on supplemental oxygen.
TLF: You have said people may not know they can make a difference. How can they do that?
BJ: They can do it by participating in clinical trials to help find a cure for LAM. They can do it by lobbying Congress to enact bills that are favorable to NIH funding and oxygen reform.
TLF: What needs to happen for SOAR to pass?
BJ: Get the attention of members of Congress. That is difficult to do because they have so many issues that are presented to them. There has to be a huge lobbying effort from everyone using oxygen to get their attention.