Management of Pneumothorax – What is the Best Strategy?
By Sandra Starnes, MD, Associate Professor of Surgery, John B. Flege Chair in Cardiothoracic Surgery, University Of Cincinnati College Of Medicine
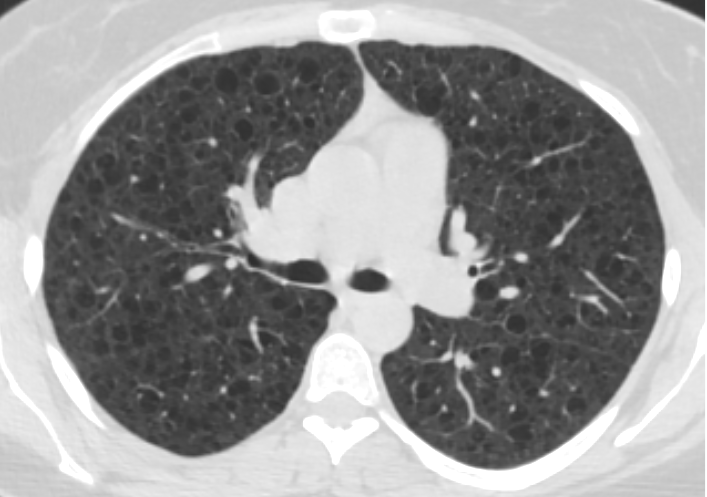
Pneumothorax (collapsed lung from accumulation of air between the lung and the chest wall) is a significant problem in patients with LAM. Up to 70% of patients will ultimately develop at least one pneumothorax in their lifetime and this is often the first sign of LAM. Most commonly, the pneumothorax occurs spontaneously without inciting factors (such as vigorous exertion). Unlike patients with Primary Spontaneous Pneumothorax (which occurs in patients without apparent underlying lung disease) who have about a 25% risk of recurrent pneumothorax after a first episode, three-quarters of women with LAM suffer from recurrence if nothing is done to prevent it. In a survey conducted from The LAM Foundation database, participants reported an average of 3.5 episodes of pneumothorax resulting in an average of one month total spent in the hospital.
There are a variety of treatment options for a spontaneous pneumothorax including simple observation, chest tube placement, chemical pleurodesis through a chest tube, and surgery. Conservative management with observation until air is naturally resorbed by the body or simple chest tube placement alone has a very high rate of recurrence (about 65%) in patients with LAM. Because of this, most thoracic surgeons recommend pleurodesis (a procedure which obliterates the pleural space to prevent future pneumothoraces) after the first episode of pneumothorax. Pleurodesis can be done mechanically (using physical abrasion) or chemically (using talc, doxycycline, bleomycin or other agents). While chemical pleurodesis through a chest tube can be successful, this may result in incomplete pleurodesis due to uneven distribution of the chemical. Surgical treatment, using video-assisted thoracoscopy (VATS), is the preferred approach. In this procedure, cameras, forceps and other instruments are inserted through fingertip-sized incisions in the chest wall, rather than through the large incisions with rib-spreading that are used in thoracotomies or open procedures. The recurrence rate after surgical pleurodesis in patients with LAM is reported to be about 25-30%; however, there are strategies to help optimize success. First, surgical intervention should ideally be performed by a thoracic surgeon (rather than a general surgeon or heart surgeon) experienced in minimally-invasive surgery, pleurodesis and LAM (if possible). An aggressive mechanical pleurodesis which involves abrading the pleural surfaces with a piece of gauze or rough pad to promote an intense inflammatory response is the most common first intervention. Resection of the offending bleb or cyst is a common part of pleurodesis for patients without underlying lung disease or those with emphysema. However, this should generally be discouraged in patients with LAM because it is often impossible to tell which cyst is the culprit and staple lines placed in LAM lung tissue may lead to prolonged air leaks that are difficult to manage.
The procedure is done under general anesthesia and it is important that the anesthesiologist be experienced with thoracic surgical procedures in patients with lung disease so that protective lung strategies are used such as maintaining low airway pressures during surgery. An epidural catheter for postoperative pain control is standard in our practice, and provides excellent post-operative pain control. The chest tube is usually kept to suction for 48 hours after surgery and the typical hospital stay is about 3 days. Most patient can return to normal activity in 2-3 weeks. Patients should avoid anti-inflammatory agents such as ibuprofen or naproxen for 3 weeks. Sirolimus should also be stopped for at least a week before surgery and for 3 weeks after surgery. These medications may prevent effective pleurodesis from occurring. In addition, patients should avoid flying for one month after surgery.
For patients with recurrent pneumothorax after surgical intervention, there are several options. For patients with a total or near total collapse, repeat surgical intervention is recommended. Options include a repeat mechanical pleurodesis if it is unclear whether an appropriate mechanical pleurodesis was done initially or pleurectomy in which the pleura overlying the ribs is actually removed. Another option to consider for refractory pneumothorax is chemical pleurodesis in which a drug or other agent is used to create an inflammatory response that results in pleurodesis. Talc is the most commonly used agent due to its effectiveness. Historically, talc pleurodesis was considered a contraindication to future lung transplantation because of the intense inflammatory response that made surgery very difficult. However, in the 2014 consensus document for the selection of patients for lung transplant by the International Society for Heart and Lung Transplantation, pleurodesis was not considered a contraindication for transplantation. They recommended that “pneumothorax in a patient who may become a future transplant recipient should be given the best immediate management… and “the choice of intervention is unlikely to affect future acceptance for transplantation.” Patients who undergo lung transplantation after a pleural intervention are at higher risk of bleeding complications; therefore, a strategy of optimizing successful treatment of pneumothorax while minimizing the impact on potential future lung transplantation should be undertaken. Given the potential that any intervention could have an impact on future lung transplantation should this become necessary, it is critical that the patient, pulmonologist and surgeon work together to develop the best treatment plan for each individual patient. It should be noted, that talc has recently become less available due to manufacturing delays and it is unclear when adequate supplies will return. Alternatives, which are generally thought to be less effective, include bleomycin, doxycycline or iodine.
References:
- Almoosa KF, Ryu JH, Mendez J, Huggins JT, Young LR, Sullivan EJ, Maurer J, McCormack FX, Sahn SA. Management of pneumothorax in lymphangioleiomyomatosis. Effects on recurrence and lung transplantation complications. Chest 2006; 129: 1274-1281.
- Weill D, Benden C, Corris PA, Dark JH, David RD, Keshavjee S, Lederer DJ, Mulligan MJ, Patterson GA, Singer LG, Snell GI, Verleden GM, Zamora MR, Gianville AR. A consensus document for the selection of lung transplant candidates – an update from the Pulmonary Transplantation Council of the International Society for Heart and Lung Transplantation. J Heart Lung Transplant 2015; 34: 1-15.